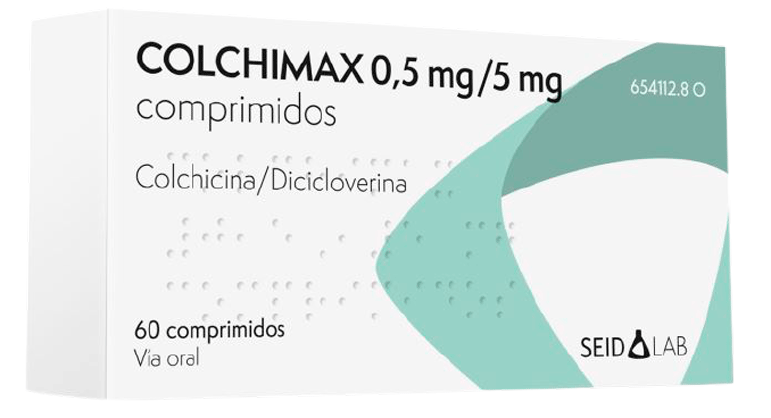
4.1 Therapeutic indications
Treatment for acute gout attacks and for chronic gout, prophylaxis of acute attacks at the start of treatment with uric acid mobilisers and periodic disease (familial Mediterranean fever).
4.2 Posology and method of administration
Colchicine has a narrow therapeutic index and is extremely toxic in case of overdose. The following dose should not be exceeded under any circumstances, as it could be fatal.
Oral administration.
The recommended dose depends on the patient’s age, renal and hepatic function and the concomitant use of other medications (see sections 4.4 and 4.5)
Adults.
Acute gout attack:
The recommended dose is 2 tablets (1 mg of colchicine) at the first sign of acute gout attack, followed by 1 or 2 tablets (0.5 to 1 mg) one or two hours after the first dose. Do not administer doses of more than 2 mg in 24 hours. Doses higher than 2 mg a day have not shown greater efficacy, but the adverse effects are increased.
This dosing regimen can be administered for up to a maximum of 4 consecutive days, with a total cumulative dose of 6 mg in 4 days. If necessary because the pain of the gout attack persists, the above-described regimen may be repeated, but always after a “wash-out period” of least 3 days without treatment.
Preventive treatment of gout attacks during initial therapy with allopurinol or uricosuric agents:
The recommended dose as preventive treatment of gout attacks is 0.5 mg of colchicine once or twice a day, which is equivalent to 1 tablet once or twice a day.
Periodic disease or familial Mediterranean fever:
The recommended dose of colchicine is 1 to 2.5 mg daily. It may be administered in two daily doses or one single dose.
Treatment of chronic gout:
The recommended dose for the treatment of chronic gout is 0.5 mg to 1 mg daily, which is equivalent to 1 tablet once or twice a day.
Children and adolescents under 18 years of age.
Acute gout attack, prevention of gout attacks and chronic gout:
There are insufficient data to make recommendations for this age group.
Periodic disease or familial Mediterranean fever:
There are insufficient data to make recommendations for this age group.
Renal impairment.
In patients with mild renal impairment (CrCl 50-80 ml/min), no dose adjustment is required (see sections 4.4 and 5.2), although close monitoring for possible adverse effects is recommended. If adverse effects do occur, it may be necessary to reduce the dose.
In patients with moderate renal impairment (CrCl 30-50 ml/min), it may be necessary to halve the dose and/or increase the intervals between doses.
In cases of severe renal impairment (CrCl < 30 ml/min), the use of colchicine is contraindicated (see section 4.3).
Hepatic impairment.
In patients with mild to moderate hepatic impairment, no dose adjustment is required (see sections 4.4 and 5.2), although close monitoring for possible adverse effects is recommended. If adverse effects do occur, it may be necessary to reduce the dose.
In patients with severe hepatic impairment, a dose reduction is necessary (see section 4.4).
Elderly patients and special populations.
In elderly patients or those with renal or hepatic impairment, alternative therapies should be used. If colchicine is to be administered to these patients, the cumulative dose over a 4-day period must not exceed 3 mg, instead of the recommended adult dose of 6 mg (see section 4.2).
4.3 Contraindications
-
-
-
-
- Hypersensitivity to the active substances or to any of the excipients of this medicinal product.
- Pregnancy.
- Severe renal impairment and haemodialysis patients.
- Glaucoma.
- Angle-closure glaucoma.
- Prostate adenoma.
- Severe gastrointestinal disorders.
- Gastrointestinal obstruction.
- Stomach ulcer.
- Severe ulcerative colitis.
- Reflux oesophagitis.
- Pyloric stenosis.
- Paralytic ileus.
- Myasthenia gravis.
- Urinary obstruction or retention due to any condition of the urinary tract or prostate.
- Cardiac disorders.
- Haematological alterations, such as blood dyscrasias.
- For 14 days after using CYP3A4 and/or P-glycoprotein inhibitors.
4.4. Special warnings and precautions for use
Special care must be taken with COLCHIMAX tablets in the following situations: Colchicine:
-
-
-
-
- If diarrhoea occurs, discontinue the medication or reduce the dose.
- In elderly patients, children and debilitated or alcoholic patients, treatment with colchicine should be closely monitored because of the increased risk of cumulative toxicity in these populations.
- Leukopenia, granulocytopenia, thrombocytopenia, pancytopenia, aplastic anaemia and myelosuppression have been associated with the use of colchicine at therapeutic doses, so it is recommended that the patient should be monitored for side effects and have regular blood tests.
- In patients with hepatobiliary and renal dysfunction, it may be necessary to adjust the dose. During treatment of the acute gout attack, the patient should be continuously monitored in case of renal or hepatobiliary dysfunction.
- Colchicine is significantly excreted in the urine in healthy individuals. Colchicine clearance is decreased in patients with renal impairment. Total body clearance of colchicine is reduced by up to 75% in patients with kidney disease undergoing dialysis (see section 5.2).
- Colchicine cannot be eliminated in patients undergoing dialysis so, a priori, its use is contraindicated (see section 4.3).
- In patients with hepatic impairment, colchicine clearance may be significantly reduced and its plasma half-life increased. In patients with severe hepatic impairment, it is necessary to reduce the dose and limit treatment to a maximum of one day every two weeks. Patients should be closely monitored to prevent serious adverse effects.
- Neuromuscular toxicity and rhabdomyolysis have been reported with chronic treatment at therapeutic doses. This risk may be increased in patients with renal impairment and in elderly patients (even those without renal and hepatic impairment).
- Concomitant use of atorvastatin, simvastatin, pravastatin, fluvastatin, gemfibrozil, fenofibrate, fenofibric acid or bezafibrate (which themselves are associated with myotoxicity), digoxin or ciclosporin with colchicine may increase the occurrence of myopathies (see section 4.5). Once treatment with colchicine is discontinued, the symptoms usually disappear within a period of one week to several months.
Dicycloverine:
-
-
-
-
- Renal or hepatic impairment.
- Autonomic neuropathy.
- Tachycardia.
- Heart failure.
- Hyperthyroidism.
- Hypertension.
- Hiatus hernia.
- Suspected or confirmed prostatic hypertrophy.
- Blurred vision.
- Somnolence.
4.5. Interaction with other medicinal products and other forms of interaction
Greater precaution should be taken when colchicine is combined with active substances that are metabolised by or interact with the cytochrome P450 system, in particular with the CYP3A4 isoenzyme or P-glycoprotein.
-
-
-
-
-
- Anti-infective agents: colchicine toxicity is increased by simultaneous treatment with clarithromycin, erythromycin or telithromycin and CYP3A4 substrates and inhibitors, particularly in patients with pre-existing renal impairment. Other CYP3A4 inhibitors, such as itraconazole, ketoconazole, indinavir, nelfinavir, ritonavir and saquinavir, may increase colchicine toxicity.
- Calcium channel blockers: verapamil and diltiazem.
- Ciclosporin: colchicine should be used with caution in combination with ciclosporin due to the possible risk of increased neurotoxicity and myotoxicity.
- Vitamins: the absorption of Vitamin B12 may be altered by chronic or high-dose administration of colchicine. Vitamin requirements may be increased.
Concomitant use of atorvastatin, simvastatin, pravastatin, fluvastatin, gemfibrozil, fenofibrate, fenofibric acid or bezafibrate (which themselves are associated with myotoxicity) may increase the occurrence of myopathies. Once treatment with colchicine is discontinued, the symptoms usually disappear within a
period of one week to several months.
Ingestion of grapefruit juice (which inhibits CYP3A4) should be avoided during treatment with colchicine, as it may increase the toxicity of colchicine.
The action of dicycloverine may be increased by drugs with an anticholinergic effect, such as tricyclic antidepressants, amantadine, class I antiarrhythmic agents (quinidine), antipsychotic agents (phenothiazine), benzodiazepines, MAOIs, narcotic analgesics (meperidine), nitrates and nitrites, antacids and sympathomimetic agents.
4.6. Fertility, pregnancy and lactation
Fertility
There are no data regarding the possible effects of colchicine on fertility. Pregnancy:
No malformations or foetal/neonatal toxicity were observed after colchicine exposure in a limited number of pregnant women with familial Mediterranean fever. However, animal studies with colchicine have shown teratogenic effects. Therefore, as a precautionary measure due to the absence of controlled studies in humans and because it crosses the placenta, with the consequent risk to the foetus due to its mechanism of action, its use during pregnancy is contraindicated (see sections 4.3 and 5.3).
Breast-feeding
Colchicine and dicycloverine are excreted in breast milk.
Colchicine is contraindicated during breast-feeding.
4.7 Effects on ability to drive and use machines
This medicine may cause drowsiness and blurred vision.
Patients who drive vehicles and use dangerous machinery are warned about this possibility.
4.8. Undesirable effects
Adverse reactions to anticholinergic drugs include the following, although not all of them have been reported with dicycloverine:
-
-
-
-
-
- Gastrointestinal disorders such as dry mouth, nausea, vomiting and abdominal pain.
- Nervous system disorders such as drowsiness, weakness and headache.
- Eye disorders such as blurred vision, diplopia, mydriasis and ocular hypertension.
- Skin and subcutaneous tissues disorders such as skin rash and urticaria.
- Urinary retention.
- Tachycardia.
- Dyspnoea.
Common adverse reactions to colchicine that have been reported include nausea, vomiting and abdominal pain. High doses may cause severe diarrhoea, gastrointestinal bleeding, skin rashes and hepatic or renal impairment.
Peripheral neuropathy, myopathy, rhabdomyolysis, alopecia and azoospermia have occurred occasionally, and with prolonged treatment there can be bone marrow failure with agranulocytosis, thrombocytopenia and aplastic anaemia.
Treatment should be discontinued and the patient should go to an emergency department at the first symptom of nausea, vomiting, abdominal pain or diarrhoea.
According to the AGREE study (see section 5.1), in which 185 patients with acute gout attack were allocated to three different treatment groups: high-dose colchicine treatment [1.2 mg followed by 0.6 mg every hour for 6 hours (total: 4.8 mg)], low-dose treatment [1.2 mg followed by 0.6 mg in the next hour (total: 1.8 mg)] and placebo treatment, the incidence of adverse reactions in the different groups was 76.9%, 36.5% and 27.1%, respectively. The incidence of the most frequently reported adverse reactions is detailed below. See Vademecum
4.9 Overdose
Colchicine has a narrow therapeutic index and is extremely toxic in case of overdose. High-risk patients are those with hepatic or renal impairment, gastrointestinal or cardiac disorders and elderly patients.
Because colchicine overdose is complex, specialist advice should be obtained rapidly to manage the overdose as promptly as possible.
The exact dose of colchicine that causes significant toxicity is unknown. Deaths have been reported after ingestion of doses as low as 7 mg over a 4-day period, while there are cases of patients who survived taking doses of more than 60 mg.
From a review of 150 overdose patients, it has been established that those who ingested a dose lower than 0.5 mg/kg survived, with a milder toxicity profile, while subjects who took doses between 0.5 and 0.8 mg/kg experienced more severe reactions, including myelosuppression. There was a 100% mortality rate in subjects who ingested more than 0.8
mg/kg.
There may be a delay of up to 6 hours before toxicity becomes apparent and some signs may even be delayed for up to a week or more. Therefore, any patient with suspected overdose, even without apparent signs, should seek specialist medical attention immediately.
The first signs of acute colchicine toxicity usually appear approximately 24 hours after ingestion. The most common symptoms include burning sensation and discomfort in the mouth and throat, difficulty swallowing, digestive disorders such as diffuse abdominal pain, nausea, vomiting, tenesmus, severe diarrhoea (in some cases bloody), resulting in dehydration (metabolic acidosis) and circulatory disorders (hypotension), which together can lead to hypovolaemic shock. Peripheral leukocytosis has occasionally been observed.
After the first 24 hours and for up to 7 days, the signs of toxicity include confusion, alopecia, cardiac disorders (including arrhythmias and decreased cardiac output), renal and hepatic impairment, respiratory distress, hyperpyrexia and bone marrow suppression. These signs may progress to multi-organ failure accompanied by bone marrow aplasia, CNS toxicity, seizures, coma, hepatocellular damage, rhabdomyolysis, respiratory distress, renal and cardiac damage and disseminated intravascular dissemination. Death is generally due to cardiorespiratory depression.
Patients who survive beyond 7 days after an overdose may experience alopecia, rebound leukocytosis and stomatitis (about 10 days after the overdose).
TREATMENT:
Treatment of colchicine overdose should include the use of oral activated charcoal in adults who have ingested more than 0.1 mg/kg of body weight of colchicine during the one-hour period following its ingestion and also in children who have ingested any amount during a one-hour period.
Higher doses of activated charcoal may increase systemic elimination and may be considered in patients who have ingested more than 0.3 mg/kg of body weight.
There is no specific antidote for colchicine. Gastric lavage may be performed. Haemodialysis and haemoperfusion do not increase the elimination of colchicine. Treatment of overdose should include general supportive and symptomatic measures depending on the patient’s clinical condition, including monitoring of vital signs, ECG, haematological and biochemical values. Breathing assistance may be required.
Circulation should be maintained and the water-electrolyte balance should be corrected.
In case of severe abdominal pain, 10 mg of morphine sulphate may be administered intramuscularly.
To aid with the management of delayed onset of symptoms, patients should be monitored carefully for at least 6 hours after overdose, or at least 12 hours if they have taken more than 0.3 mg/kg of body weight. After this time, asymptomatic patients can be discharged with the warning that if they notice gastrointestinal symptoms, they should return to the unit where they were treated.
The signs and symptoms of dicycloverine overdose include headache, nausea, vomiting, blurred vision, dilated pupils, sensation of heat, dry skin, vertigo, dry mouth, difficulty swallowing and central nervous system stimulation.
The amount of dicycloverine administered in a single dose that is associated with symptoms of overdose has not been defined. The maximum oral dose recorded in adults was 1500 mg and the adult survived.
Treatment of overdose consists of gastric lavage, administration of emetics and activated charcoal. Sedatives may be administered to treat excitatory symptoms.